Written by Carley B Alves, BS MS, Assistant Fitness Manager, Marilyn Fox Building
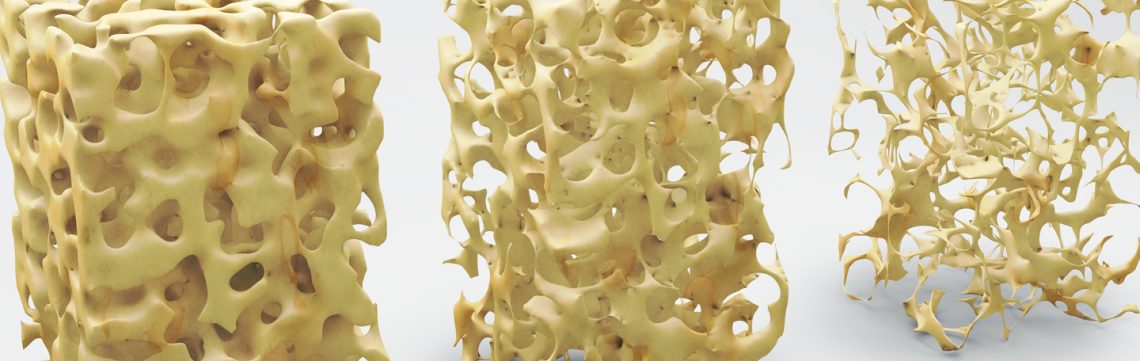
“Osteoporosis is a disease resulting in decreased bone mass and microdamage to bone structure which increases susceptibility to fracture1.”
May is National Osteoporosis Month, so we wanted to offer some insight into the disease since it affects so many of us, both young and old. Let’s explore the myths and facts and discuss a few tips to reduce the risk of developing it and how to increase bone density once diagnosed.
Myths
- Most people do not need to worry about osteoporosis.
- People with osteoporosis can feel their bones getting weaker.
- Osteoporosis is not a serious condition.
- If you drink milk and take calcium you won’t get osteoporosis.
- There is nothing I can do about it.
Facts
- 44 million Americans have been diagnosed with low bone density or osteoporosis.
- 1 in 2 women and up to 1 in 4 men, over the age of 50, will break a bone due to osteoporosis.
- Young women can get exercise or diet induced-osteoporosis from overtraining & poor diet.
- Osteoporosis is a silent disease: fracture or loss of height are often the first signs.
- 24% of patients 50 years or older with a hip fracture die after one year from complications.2
Risk Factors for Osteoporosis are varied.
- Personal or family history of fractures
- Family history of osteoporosis
- Fall history associated with diseases such as Dementia, Stroke, Epilepsy
- Steroid use
- Tobacco use
- Alcohol use
- Caffeine intake
- Low body weight
- Excessive or long-distance cardiovascular exercise, along with very low body fat
- Inadequate physical activity, i.e. spend most of waking hours sitting
- Menopause (women lose up to 20% bone density five years after onset of menopause)
- Age 50+
- Poor health
- Dietary issues such as Calcium or Vitamin D deficiency3
- Eating Disorders such as Anorexia and Bulemia
- Kidney Disease
- Hyperthyroidism1,2,4
If you have several of the risk factors listed, you might consider getting tested for osteoporosis or osteopenia. Osteopenia is the precursor to osteoporosis. If you catch it early, it is often reversible, or you can at least halt the progressive decrease in bone density if you do nothing. I have worked with several clients who had osteoporosis and asked to see their test results. Then after working with them on an exercise program for one year, I’d request they receive another bone density test to find that their bone density increased and reverted from osteoporosis to osteopenia!
Testing for osteoporosis is simple. Your primary physician or internal medicine doctor should be able to perform a bone density test. A DXA is more accurate than a plain x-ray4. They usually order scans for your hip, spine and sometimes wrist and/or forearm. If one hip is bothering you more than the other, ask to have that side scanned as they usually do not do both. The scan is simple and pain-free. Usually if diagnosed with osteoporosis, they will advise that you return the following year for another scan after making recommendations for treatment.
My personal story begins with my grandmother who had a hip fracture from which she never fully recovered. She was diagnosed with both Alzheimer’s and osteoporosis and lived until she was 99, but the last 10 years of her life were in a wheelchair. My sister has been diagnosed with osteopenia. I myself have osteopenia in my hip. My mother has had osteoporosis for the past 10 years and is 94 years old. She took Boniva, a prescription drug, for a while and is on vitamin D and calcium supplements. She has been told to exercise, but she also has dementia and does not remember or understand why she has to exercise. As a result, she is deteriorating, losing muscle mass and falls frequently. In 2018, she has broken her wrist and foot. She spends most of her time in bed or inside, so it is not a matter of if, but when she will need a wheelchair. It is sad.
As you can see, osteoporosis runs in our family and is genetic to the females. I take a vitamin D supplement, spend time in the sun, and exercise – hiking, walking and strength training. You can be proactive about preventing osteoporosis or reversing its progression with exercise and diet. Try to incorporate weight-bearing exercises into your daily routine and minimize your caffeine intake!
Next week we will discuss fall prevention in the elderly and exercise for all ages.
- Goodman C, Fuller K, Boissonnault W. Pathology: Implications for the Physical Therapist. 2nd Philadelphia, PA: Saunders; 2003:871-882.
- National Osteoporosis Foundation. Available at: http://www.nof.org. Accessed January 2012.
- Huey, Way Review of Calcium and Vitamin D for Osteoporosis. September 2, 2014.
- St Luke’s Hospital Osteoporosis Program materials: August 4, 2014